Over the last few months, we have been seeing a lot of patients in the clinic with heartburn. This common condition is medically known as Gastroesophogeal Reflux Disease (GERD). A recent study estimated that up to 20% of Canadians will experience heartburn symptoms at least once a week (1). Many people will put off dealing with GERD, but it can have a big impact on quality of life as well as potentially some long-term consequences if left untreated.
What causes GERD:
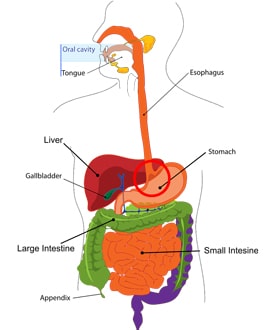
When functioning normally, our digestive system moves in one direction – down. We have multiple sphincters along the way that, along with the smooth muscle of the digestive tract, control the direction and flow of the food and liquids that we consume. In GERD, the sphincter between the esophagus and the stomach called the lower esophageal sphincter or LES (red circle in the picture) relaxes inappropriately. This allows the acidic contents of the stomach to travel backwards, up into the esophagus leading to the symptoms of GERD. There are numerous reasons why the LES may not be functioning properly, and many of them are modifiable. These include: excess abdominal weight, hiatal hernia, smoking, meal timing, stress, nutrient deficiencies, hypochlorhydria (low stomach acid), and food sensitivities.
Symptoms:
The classic symptoms of GERD are the burning sensation in the chest (“heartburn”) and regurgitation of stomach contents. The severity can range from completely painless and undetectable, to excruciating chest pain that feels like a heart attack. Some other symptoms include:
- Sour taste in mouth
- Burping
- Nausea or vomiting
- Cough, sore throat or hoarse voice
- Difficulty swallowing or sensation of a lump in your throat
- Difficulty sleeping or interrupted sleep
- Weight loss
Occasionally, people will have “silent GERD”. In these cases, the symptoms of burning and regurgitation are absent and other symptoms like cough, throat clearing, hoarse voice and “lump in throat” predominate.
What to do about GERD:
Diet changes
Certain foods seem to worsen or cause GERD symptoms including:
- Tomatoes
- Citrus fruits and juices
- Fatty or fried foods
- Alcohol, particularly red wine
- Caffeinated drinks including coffee, tea, pop
- Raw garlic, onions, black pepper and other spicy foods
- Chocolate
- Peppermint
Other foods that can cause heartburn are dairy, gluten and sugar. If you are suffering from heartburn, keep a food and symptom log to identify which foods seem to be triggers for you. Once these foods are identified, they should be avoided while treating the GERD. This doesn’t mean you will never be able to eat these foods again but while undergoing treatment, it’s best to avoid them.
How we eat can be just as important as what we eat!
Mindfulness has been a trending topic in the last few years and it can be applied to eating as well. If you are working, distracted or stressed while eating, your nervous system is not in a state where digestion is prioritized. This can cause or increase GERD symptoms.
Take a break from whatever else is going on while you are having a meal. Avoid doing work, answering the phone or emails, or scrolling through Facebook. When possible, eat at a table rather than your desk, in front of the TV or in the car. Before you begin your meal, take 3-5 deep belly breaths as this will help you get into the present moment and switch your body into parasympathetic (“rest and digest”) mode.
Also, pay attention to how fast you are eating. If you are having difficulty eating slowly, put your utensil down between bites. This can slow down your eating and allow you to get better signals from your body on when you are full. Over eating can increase GERD symptoms and frequency. Sometimes smaller, more frequent meals can help.
Finally, make sure you are enjoying your food! Notice the colours and the smells of your food before you put it in your mouth. Pay attention to the tastes and textures while you are chewing. This will keep you in the present moment as well as allow you to have a better food experience! Use this checklist as a tool to assess if you are eating mindfully.
Mindful Eating Checklist
- Am I at a table?
- Eating fast or slow?
- Have I tasted my food?
- What emotions am I feeling?
- Multitasking or focusing on my meal?
- Mindlessly munching or aware of each bite?
- Ask “How hungry am I?” on a 1-10 scale
If you find that your symptoms are keeping you up at night, try not to eat within 2-3 hours of bed, and don’t lie down after a meal as this can worsen symptoms. For more sleep tips, check out our Sleep Hygiene blog.
Supplements
If diet changes and eating habits alone are not fully resolving GERD symptoms, certain supplements can be used to soothe mucus membranes, promote healing and treat the underlying disorder.
- Deglycyrrhizinated licorice (DGL) – Often chewable, this licorice extract soothes the esophagus and stomach lining. This particular form is important because the component of licorice that can potentially increase blood pressure has been removed, making it safe for most people.
- D-Limonene – This is an extract from citrus oil. Although the mechanism for how D-limonene helps with GERD has not been fully elucidated, it may act as an acid neutralizer and help establish normal peristalsis (2).
- Magnesium – If the LES isn’t functioning properly, low magnesium may be a cause. Magnesium also has a role in other contributors to GERD especially stress.
- Melatonin – Usually when we are talking about melatonin, it is in the context of sleep. However, the GI tract contains up to 400x more melatonin than the pineal gland in the brain. Recent studies have demonstrated positive outcomes in patients taking melatonin, even when compared to PPI therapy (3).
There are many another supplements that may help with GERD including Zinc, probiotics, digestive enzymes, and Aloe, just to name a few. Determining the cause is always the key step in formulating the most effective treatment plan. This is where it is important to get the assistance of someone trained to use these products, as well as in nutrition.
Other
Spinal and visceral (organ) manipulation has been shown to have a positive effect on GI complaints, including GERD (4). When other treatments have not been effective or not as effective as desired, this could be a reasonable option to pursue.
Medications
There are many pharmaceutical options for the treatment of GERD. Antacids (ex. Tums), alginates (ex. Gaviscon®) or over the counter H2-blockers are often the first-line treatment by medical doctors and pharmacists when symptoms are mild or infrequent (5). When symptoms are more frequent or severe, proton pump inhibitors (PPIs) are the standard of care (5). These drugs often offer rapid relief to patients as they will reduce stomach acid production. Long term adverse effects of PPIs include long bone fractures, hypomagnesaemia, infections and interactions with other medications (6). There are conflicting studies on the actual risk of developing these conditions and more research is needed to understand the long term consequences. As with any prescription, a careful explanation of the risks and benefits is important. Also, according to the medical literature, these drugs are often over-prescribed, so take this into consideration when continuing this prescription (6).
When does GERD need to be further investigated?
Our stomachs are designed to deal with the low pH of stomach acid – the esophagus is not. The continual exposure of the esophagus to stomach acid can lead to further complications. The tissue of the esophagus can scar, causing esophageal strictures that can make swallowing difficult. Like the stomach, the esophagus can develop ulcers. These can be painful, bleed and make swallowing difficult. The most noteworthy GERD complication is Barrett’s esophagus, where the cells of the esophagus change due to the exposure to stomach acid. This is a precancerous condition and while progression to esophageal cancer is rare, it may be important to get an endoscopy to look for these changes. This would be especially important in someone who has had untreated GERD for a long time (>10 years) and is having other symptoms including difficulty swallowing, weight loss and vomiting blood or black tarry stool (5).
Some final thoughts
A recent article stated, [su_quote]“…medical management of GERD is not a substitute for a healthy lifestyle including maintaining a normal BMI, thorough diet and exercise, moderation of alcohol intake, and avoidance of smoking” (6)[/su_quote] This statement also applies to any supplement based management of GERD. Any prescription, whether supplements or drugs, should always be in addition to appropriate lifestyle modification and education. If you have been suffering with heartburn or GERD, it may be time to see someone. The naturopathic doctors at Horizons Holistic Health Clinic would be happy to help you soothe the burn.
Disclaimer: This information is provided for educational purposes only. Please consult a medical practitioner regarding the applicability of any opinions or recommendations with respect to your symptoms or medical conditions.
References:
- Canadian Digestive Health Foundation Public Impact Series: Gastroesophageal reflux disease in Canada: Incidence, prevalence, and direct and indirect economic impact. Fedorak RN, van Zanten SV, Bridges R. 2010, Can J Gastroenterol., pp. 24(7):431-434.
- D-Limonene: Safety and Clinical Applications. Sun, Jidong. 3, 2007, Alternative Medicine Review, Vol. 12.
- The potential therapeutic effect of melatonin in gastro-esophageal reflux disease. Kandil TS, Mousa AA, El-Gendy AA, Abbas AM. 7, 2010, BMC Gastroenterology, Vol. 10.
- What effect does chiropractic treatment have on gastrointestinal (GI) disorders: a narrative review of the literature. Angus K, Asgharifar S, Gleberzon B. 2015, The Journal of the Canadian Chiropractic Association, Vols. 59(2):122-133.
- Canadian Concensus on the management of GERD. Armstrong. 1, 2005, Can J Gastroenterol, Vol. 19, pp. 15-35.
- Clinical Implications of Emerging Data on the Safety of Proton Pump Inhibitors. Felice Schnoll-Sussman, Philip O. Katz. 1, 2017, Current Treatment Options in Gastroenterology, Vol. 15, pp. 1–9.
Share This Post!
One Comment
Comments are closed.




[…] hypertension (high blood pressure) and seizures2. In addition, the coffee can impact sleep quality, cause heartburn and raise blood cholesterol. A research group did a study on adolescents and caffeine and the […]